Abstract
Background The new Molecular International Prognostic Scoring System (IPSS-M) for myelodysplastic neoplasms (MDS) has been recently developed by Bernard et al. 2022, and considers hematologic, cytogenetic, and somatic gene mutation parameters. This study aimed to use the IPSS-M for risk assessment in Czech patients with MDS and to compare stratification of the IPSS-M with the IPSS-R.
Methods The data from 363 untreated patients with MDS were re-analyzed using the IPSS-M. Diagnoses were made according to the standard criteria. Patients who underwent hematopoietic cell transplant were censored at the time of transplant. All samples and clinical data were collected with patient consent under an Institutional Scientific Board approved protocol in accordance with the ethical standards of the Declaration of Helsinki. The IPSS-M scores were calculated as described by Bernard et al. 2022 using algorithm in the R package. Targeted gene sequencing was performed using Illumina TruSight Myeloid Sequencing Panel Kit. GraphPad Prism 7 Software was used to perform a Kaplan-Meier survival analysis.
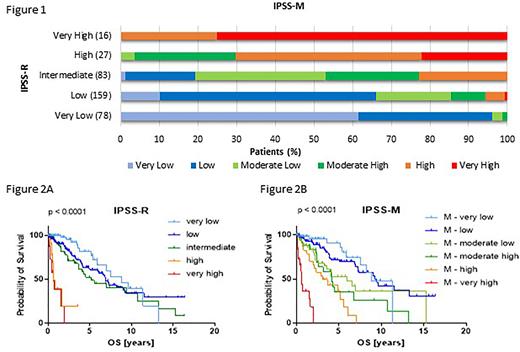
Results The median age of the cohort was 64 years, and the median follow-up was 1.8 years. Overall survival (OS) was available for 98.6 % of patients. A total of 64 % of patients had at least one pathogenic mutation. Out of these patients, 61 % carried more than 1 mutation. The number of mutations ranged from 0 to 9 per patient with a median of 1 mutation. The most affected gene was SF3B1, mutated in 26 % of mutation-positive patients. Eighty four percent of mutation-positive patients had mutation in the 16 main effect genes. The IPSS-R categories were as follows: 21% of the patients had very low, 44% had low, 23% had intermediate, 7% had high, and 4% had very high risk. Upon restratification using the IPSS-M, 18% of patients were scored as very low, 36% were scored as low, 17% were scored as moderate low, 12% were scored as moderate high, 12% were scored as high, and 5% were scored as very high risk. A total of 42% of patients were restratified into different risk categories, 71 % were upstaged and 29% were downstaged (Fig. 1). Six percent of patients from the IPSS-R low category shifted to the IPSS-M high/very high category. With a median follow-up of 1.8 years (range, 0.2-16.3 years), the median OS per IPSS-R scoring system was 8.8, 6.9, 5.2, 0.6, and 0.6 years for very low, low, intermediate, high, and very high, respectively (P<0.0001) (Fig. 2A). The median OS per IPSS-M scoring system was 8.8, 9.5, 6.0, 4.2, 3.1, and 0.6 years for very low, low, moderate low, moderate high, high, and very high, respectively (P<0.0001), (Fig. 2B). Notably, the median OS of patients in the IPSS-M high category was significantly longer compared to that in the IPSS-R high category.
Conclusions Overall, nearly half of MDS patients were restratified (mostly upstaged) in the IPSS-M. Compared to the IPSS-R, the IPSS-M improved prognostic discrimination of MDS patients, especially in patients at high and very high risk. Importantly, the new system identified patients at high/very high risk in the IPSS-R low category who may have a higher likelihood of progression and should be treated appropriately. Our study supports the concept that the incorporation of mutational data into current prognostic scoring system enhances its ability to predict the outcome in MDS patients.
Supported by AZV (NV18-03-00227) and (NU21-03-00565), GA CR (N20-19162S), and MH CZ-DRO (UHKT, 00023736).
Figure 1. Restratification of IPSS-R to IPSS-M for 363 MDS patients.
Figure 2. (A) Overall survival by IPSS-R, (B) Overall survival by IPSS-M.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.